Abstract
Purpose: As HCT recipients are at risk for late effects, SCPs are increasingly being used in clinical practice to facilitate survivor care despite the lack of high-quality data on their implementation or efficacy. We conducted a randomized study to evaluate the impact of SCPs on HCT survivors' confidence in survivorship information (CSI), with secondary analyses evaluating cancer treatment distress (CTXD), knowledge of transplant exposures, health behaviors, health care utilization (HCU) and health general self-efficacy.
Methods: Adult (≥18 yrs at HCT) survivors who were 1-5 years post-transplant, proficient in English, and without relapse or second cancers were eligible. To enhance generalizability, recipients with any diagnosis, HCT/donor type, and conditioning regimen could participate. Treatment summaries were generated using patient-specific clinical data submitted by transplant centers to the Center for International Blood and Marrow Transplant Research (CIBMTR). Focus group feedback from patients/caregivers, HCT physicians/nurses/social workers and general hematologist-oncologists informed the design of paper-based SCPs. Individualized SCPs were developed based on patient risk-factors and treatment exposures (e.g., age, sex, HCT type, graft-versus-host disease [GVHD], and use of total body irradiation [TBI] or steroids) and published guidelines for long-term followup of HCT survivors (Majhail et al, BBMT 2012). A baseline phone survey was conducted after enrollment and included standardized patient-reported outcomes (PROs) related to the objectives listed above. Patients were then randomized to SCP or routine care (RC) per their transplant center. A phone survey 2 weeks later assessed health literacy for patients on both arms and asked questions related to use of SCP for patients on the intervention arm. End-of-study phone PRO surveys were then administered at 6 months. The study was powered to detect a standardized effect size of ≥0.3 for the intent-to-treat primary outcome of CSI.
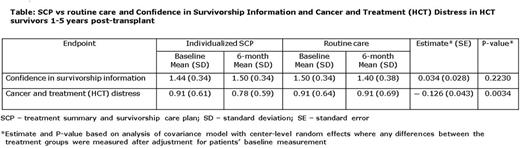
Results: A total of 495 patients were enrolled at 17 transplant centers, of whom 458 completed baseline survey and were randomized (SCP=231, RC=227); 201 (87%) SCP and 199 (88%) RC patients completed 6 month assessments. Patient and transplant characteristics (including health literacy scores) were well balanced between the two arms. Median age was 59 yrs in both arms; 96% (SCP) and 92% (RC) patients were White, 49% and 60% were male, 48% and 44% had received allogeneic HCT, 11% and 16% had received a previous HCT, and 21% and 20% had received TBI based conditioning, respectively. Among allogeneic HCT recipients, 63% and 67% had a history of acute GVHD and 60% and 66% had a history of chronic GVHD, respectively. Receiving a SCP was not associated with a change in CSI, but was significantly associated with reduction in CTXD after Bonferroni correction for multiple outcomes (Table). Decrease in CTXD score in the SCP arm was independent of sex, transplant type, GVHD status, diagnosis, and health literacy. Age was significantly associated with CTXD scores (with higher distress among younger patients), although not with the SCP effect size (no significant interaction). No SCP effect was observed on any of the other secondary outcomes.
Summary: In this large multicenter randomized study, we demonstrate that SCPs generated automatically using a centralized clinical registry (CIBMTR) to individualize to patient risk-factors, without clinical contact to interpret or personalize the SCP, is feasible and can produce a tool that lowers CTXD scores at 6 months in HCT survivors. Our study supports further development and implementation of individualized SCPs in this population that is at significant risk for late morbidity and mortality from transplantation.
Majhail: Anthem, Inc.: Consultancy; Sanofi: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal